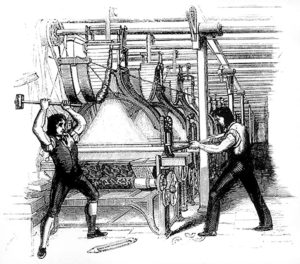
The industrial revolution began with the cloth weavers and only later transformed life for blacksmiths and longshoremen. Many people today work in textiles, manufacturing and shipping, but the way they work would bewilder their colleagues teleported from 1700. Technology vastly increased the amount of “stuff” one worker can produce, and society as a whole has reaped that benefit.
Just so, the digital revolution began with bankers and booksellers before spreading to hotels and taxis. Health care has so far, mostly, stood apart. We don’t much use papers charts anymore (even that hasn’t changed everywhere), but the basic work is all the same. However, health care’s revolution is finally upon us. In 2035, doctors will still be diagnosing and treating patients. The way they do it will have changed dramatically, and the impact a single physician can have would astound our mentors and forebears.
The future of medicine is digital
A couple doctors recently mused in JAMA about developing a new medical specialty. The “virtualists” will be specifically trained in digitally delivered medicine while everyone else sticks to their bricks & mortar. This analysis is spot on…except the paradigm will be just the opposite. Most medicine will be digital, and those who practice in person, in the ICUs and ORs, will be the specialists. We will not have any “virtualists” because we will just call them “doctors.”
For all its promise, telemedicine as practiced today is just the infancy of digital medicine. Avoiding the commute and the waiting room is great, but a revolution it is not, yet.
The revolution in digital medicine unfolding now will bring two great transformations:
1. Continuous remote care
First, the paradigm of “see the doctor every so often” that dates from at least the time of Hippocrates himself will be transformed, finally, by continuous remote care. Especially for managing chronic disease, the old paradigm, whether in person or via conventional telemedicine, is sadly ineffective as evidenced by the generally inexorable worsening of diabetes, hypertension and the like. Those fifteen minute doctor visits every few months cannot help when patients make decisions about their lifestyle every few minutes. Remote care, continuously available from a team of providers, can. Continuous remote care matches medical support with the time scale of events, and provider teams, gradually supported more and more by artificial intelligence, will meet what today is a vast unmet patient demand for real time medical advice.
This vast unmet patient demand for real time medical advice stretches across the spectrum of ages and diagnoses. As a pediatric resident, I was routinely astounded by the parents of children with chronic conditions like cerebral palsy. They knew and did everything for their children’s care in part because our medical system had no way to support them. Continuous remote care from provider teams offers a new way, finally. Mental health is already shifting to continuous care, as evidenced by the growth of services like Ginger.io and Talkspace, and Virta Health provides continuous care for patients with metabolic syndrome.
2. Digitalization of medical data
Second, digitization of both medical data and evidence based medicine will allow physicians to treat patients much more efficiently than today. The industrial revolution dramatically increased the productivity of amenable processes while leaving the rest increasingly expensive in relative terms. Clothing and cooking pans are much, much cheaper than they were in 1700 while the services of barbers, physicians and the like have gotten even costlier.(1) The digital revolution will finally increase productivity in medical services. And not a moment too soon as societies, particularly in the US, struggle to provide widespread access to decent health care without going bankrupt.
The need for some human judgment and human touch may not disappear any time soon, if ever. Artificial intelligence must be employed with great caution in assisting medical decisions, but its scope to improve patients’ access to quality care is transformational.
- The great economist William Baumol called this concept cost disease. After my mentor Bill Meehan, I like calling it “the symphony problem”. A live performance of Mozart’s 40th requires exactly as much human effort in 2017 as it did when it was written in 1788 while producing the clothing, food and transportation for the orchestra has gotten tremendously cheaper.
